Online Communities
ADHD in the News 2026-01-22
January 22, 2026In Good Health: What we know about ADHD
Busting ADHD Myths at APSARD
Youth ADHD Treatment Barriers and Outcomes: Insights from APSARD
ViewJanuary 22, 2026
January 22, 2026Moving Forward After Job Loss
Help Your Teen Plan a Rewarding Gap Year
Using Cultural Humility to Engage Black Families About ADHD
ViewEvents
-
Understanding Family Perspectives to Better Support Black Children With ADHD Ask The Expert
February 4, 2026 | 2:00 PM
Register -
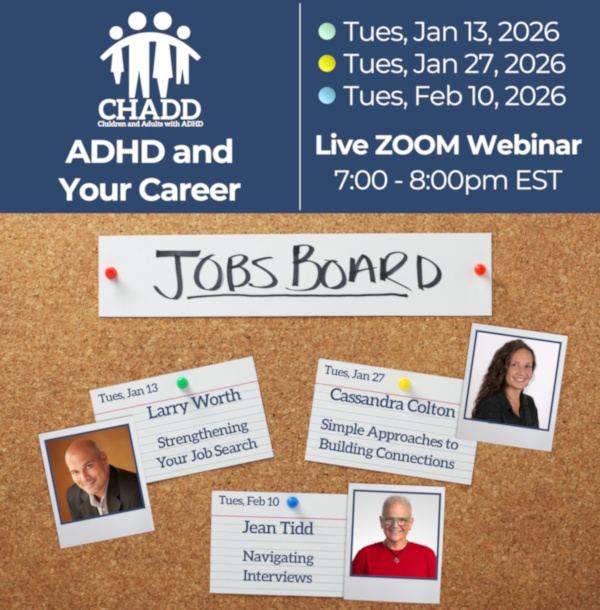
ADHD and Your Career: Navigating Interviews
February 10, 2026—February 10, 2026 | 7 PM ET
Register -
Training on ADHD | Self-Paced Online Courses
November 1, 2024—November 1, 2034
Register -
Listen to podcasts about ADHD
December 1, 2025—November 1, 2034
Register -
ADHD and Your Career: Simple Approaches to Building Connections
January 27, 2026—January 27, 2026 | 7 PM ET
Register -
ADHD and Your Career: Strengthening Your Job Search
January 13, 2026—January 13, 2026 | 7 PM ET
Register
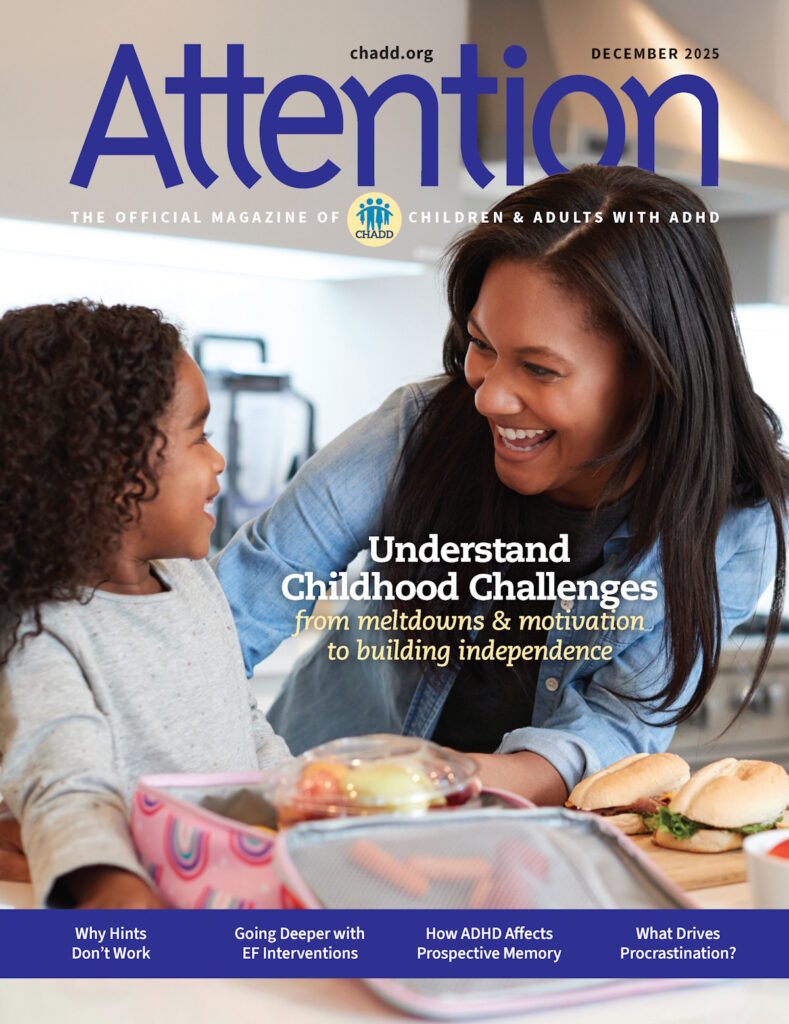
Attention Magazine
Recognized for its excellence, CHADD’s bimonthly magazine is rich in practical information, clinical insights, and evidence-based strategies for managing ADHD.
LEARN MORE